Overview
The 7mm rule. What to do when your uterine lining refuses to thicken before transfer.
If you’ve been through even one fertility cycle, you know this obsession well.
Every scan begins with the same question.
How’s the lining?
The number appears. 5.8 mm. 6.2 mm. 6.7 mm.
And suddenly everything else fades into the background.
Good embryos don’t matter anymore. Hormones don’t matter. Effort doesn’t matter.
Only the lining does.
And when it stays thin, cycle after cycle, the fear sets in quietly.
Is my body failing me?
Is this the reason nothing is working?
Let’s talk about this honestly, without panic and without false reassurance.
What “Thin Endometrial Lining” Actually Means
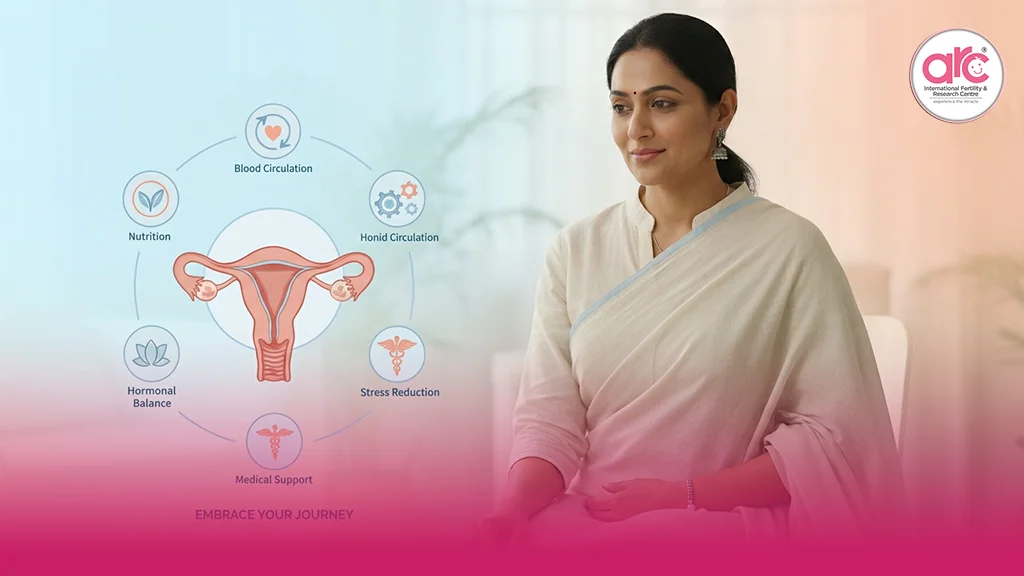
The endometrium, your uterine lining, is where implantation happens. It thickens under estrogen, matures under progesterone, and ideally becomes soft, vascular, and receptive.
Clinically, most fertility specialists look for a minimum lining for embryo transfer of around 7 to 8 mm, with a trilaminar pattern. That number isn’t magic, but it exists for a reason. Implantation rates drop noticeably below it.
A thin endometrial lining doesn’t mean pregnancy is impossible. But it does mean the odds are working against you, especially in IVF cycles where timing is everything.
At a fertility hospital in Chennai, thin lining is one of the most emotionally distressing issues patients face, not because it’s rare, but because it feels uncontrollable.
Why Some Linings Refuse to Thicken
A thin lining is not laziness. It’s information.
It can reflect:
- Poor uterine blood flow
- Chronic inflammation or scarring
- Low estrogen response
- Previous uterine procedures
- Hormonal imbalance
- Conditions like Silent Endometriosis, which can quietly affect receptivity without pain
The lining doesn’t thin without a reason. It’s responding to its internal environment.
Which means improving it isn’t about forcing thickness. It’s about changing the conditions that allow it to grow.
The 7mm Rule, and Why It Causes So Much Anxiety
Patients obsess over numbers because numbers feel concrete.
But here’s the nuance most people aren’t told. Thickness alone is not the whole story. Blood flow, pattern, and timing matter just as much.
Still, when the lining refuses to cross 7 mm, doctors pause transfers for a reason. Implanting into an unreceptive lining is not optimism. It’s gambling.
The best fertility hospital in Chennai doesn’t cancel cycles casually. It does it to protect embryos, not punish patients.
5 Ways Doctors Try to Improve Endometrial Receptivity
This is where strategy replaces panic.
1. Improving Blood Flow, Not Just Hormones
Estrogen builds the lining, but blood flow sustains it. Poor circulation means even high estrogen won’t work well.
This is why doctors often recommend supplements like Vitamin E and L-arginine, which support vascular dilation and oxygen delivery. These aren’t miracle pills. They’re tools to improve the environment, not override it.
Gentle movement, warmth, and reducing pelvic tension matter more than people realise.
2. Correcting Inflammation Before Pushing Thickness
Inflammation makes the uterus defensive.
Chronic, low-grade inflammation can prevent the lining from responding, even when hormones are adequate. This is why some women show stubborn thin linings despite “good” estrogen levels.
In such cases, addressing infection, inflammation, or conditions like silent endometriosis becomes more important than increasing doses blindly.
3. Adjusting Estrogen Delivery, Not Just Dose
More estrogen isn’t always the answer.
Some women respond better to patches than pills. Others need vaginal or injectable routes. It’s not about quantity, it’s about how the body absorbs and uses it.
When doctors change the route instead of the dose, linings sometimes respond for the first time.
4. PRP, When the Lining Needs Regeneration, Not Stimulation
For women with persistently thin linings, especially after surgeries or repeated failed cycles, PRP (Platelet-Rich Plasma) has emerged as a supportive option.
PRP uses your own blood-derived growth factors to stimulate healing and tissue regeneration. It doesn’t force thickness overnight. It encourages the lining to behave like healthy tissue again.
PRP is not for everyone. But when used selectively, it can shift the lining from resistant to responsive.
5. Testing Timing, Not Just Thickness
Sometimes the lining isn’t thin. It’s mistimed.
This is where the ERA test for IVF success enters the conversation. ERA doesn’t measure thickness. It assesses when the lining is actually receptive.
Some women have a perfectly adequate lining that simply isn’t ready on the assumed transfer day. Adjusting progesterone timing can dramatically improve outcomes without changing thickness at all.
Why Obsessing Over Millimetres Can Be Misleading
A 6.9 mm lining with excellent blood flow may implant better than an 8.2 mm lining that’s inflamed and poorly vascularised.
Thickness is a threshold, not a guarantee.
What matters is receptivity, not just measurement.
The Emotional Weight of a Thin Lining
Thin lining hits differently.
It feels personal. As if the uterus itself is refusing. As if the body isn’t cooperating despite effort.
But the lining isn’t stubborn. It’s cautious.
It needs safety, blood flow, hormonal clarity, and time.
What You Need to Remember
A thin endometrial lining is not a verdict.
It is a message.
It’s asking for better conditions, not more pressure.
When doctors pause a cycle to improve the lining, they’re not delaying your future. They’re protecting it.
And when the lining finally responds, slowly, quietly, often after months of frustration, it reminds you of something important.
The uterus doesn’t rush.
It prepares.
And when preparation is respected, implantation becomes possible again.