Overview
You’ve done everything asked of you.
You’ve shown up for scans.
You’ve trusted the protocol.
You’ve endured injections you never imagined giving yourself.
And now you’re sore. Bruised. Exhausted.
So the question slips out, half-whispered, half-guilty.
Can I stop the Progesterone in Oil shots and switch to suppositories… without risking my pregnancy?
If you’re searching progesterone oil vs suppositories IVF, you’re not being lazy. You’re being human.
Let’s talk about this properly. Without fear tactics. Without outdated dogma.
Why Progesterone Matters So Much in IVF
Progesterone is not optional in IVF. It’s foundational.
In a natural cycle, the ovary produces progesterone after ovulation to stabilise the uterine lining. In IVF, especially frozen embryo transfers, the body often doesn’t produce enough on its own.
Progesterone:
- Prepares the lining for implantation
- Supports early pregnancy
- Reduces uterine contractions
- Maintains the environment until the placenta takes over
Low progesterone doesn’t just affect implantation. It can increase early pregnancy loss.
That’s why clinics take it seriously.
At a fertility hospital in Chennai, progesterone support is never casual. But how it’s given has evolved.
PIO Injections: Why They Became the Gold Standard
Progesterone in Oil, or PIO, has been used for decades.
It’s injected deep into muscle, usually the glute. It creates high, stable blood levels of progesterone. For a long time, this reliability made it the default choice.
Doctors trusted it because:
- Blood levels were predictable
- Absorption was consistent
- Early studies showed good pregnancy outcomes
But reliability came at a cost.
Pain. Inflammation. Lumps. Nerve irritation. Months of daily injections that turn bodies into pincushions.
So when women ask to switch, the fear isn’t about convenience. It’s about safety.
Vaginal Progesterone: Not the “Weaker” Option People Think
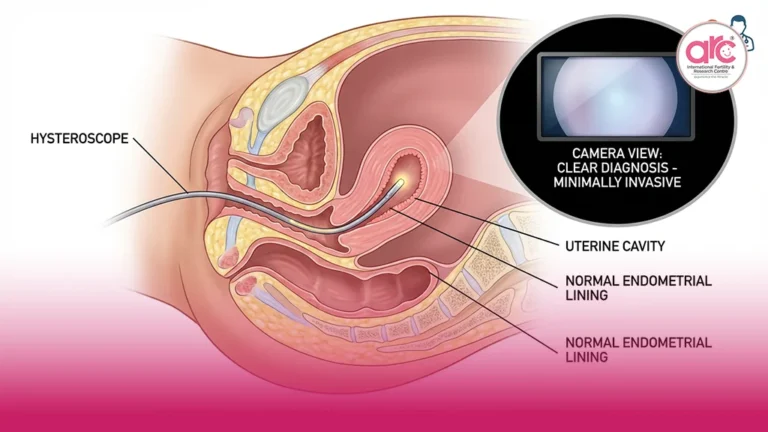
Progesterone pessaries, gels, or capsules are absorbed directly through the vaginal tissue into the uterus.
Here’s the part most people don’t realise.
Vaginal progesterone creates higher progesterone levels in the uterus, even if blood levels appear lower.
This is called the “first uterine pass effect.”
In other words, what matters most, progesterone at the implantation site, can be very well supported with vaginal routes.
What 2026 Clinical Data Actually Shows
This is where outdated fear lingers longer than evidence.
Large studies and updated meta-analyses up to 2026 show that for frozen embryo transfer (FET) cycles:
- Vaginal progesterone and PIO injections have similar implantation rates
- Ongoing pregnancy and live birth rates are comparable
- Miscarriage rates do not significantly differ when progesterone levels are adequate
The key phrase there is when progesterone levels are adequate.
It’s not about the route alone. It’s about whether your body is actually getting enough support.
This is why the best fertility hospital in Chennai doesn’t use a one-size-fits-all rule anymore. Monitoring and individual response matter more than tradition.
Why Some Clinics Still Insist on PIO
Part of it is habit.
Part of it is fear of change.
Part of it is concern about patient compliance with vaginal dosing.
And part of it is that some patients genuinely absorb progesterone better through injections.
The mistake is assuming that everyone needs the same route to be safe.
They don’t.
When PIO Might Still Be the Better Choice
Let’s be clear. PIO is not obsolete.
PIO may be preferred if:
- Progesterone levels remain low on vaginal support
- There is repeated implantation failure
- There is a history of early pregnancy loss linked to low progesterone
- The patient struggles with vaginal absorption
Sometimes, clinics use combination therapy, lower-dose PIO with vaginal progesterone, to reduce injections while maintaining levels.
This is not compromise. It’s optimisation.
When Switching to Suppositories Is Usually Safe
Switching is often reasonable when:
- Progesterone blood levels are stable
- The pregnancy is progressing well
- There is no prior progesterone-related loss
- The patient is experiencing significant injection-related pain or inflammation
This decision should always be made with monitoring, not guesswork.
That’s the difference between fear-driven protocols and evidence-based care, something explored deeply in Why Couples Prefer Fertility Hospitals in Chennai for Advanced Treatments?
What Actually Prevents Miscarriage
This part needs to be said clearly.
Progesterone supports pregnancy.
It does not control chromosomal fate.
It does not override genetic abnormalities.
Many early miscarriages are due to embryo genetics, not progesterone route.
So switching from PIO to suppositories does not suddenly “cause” miscarriage if progesterone levels remain adequate.
Blaming route changes for losses often creates unnecessary guilt.
The Emotional Cost of Staying Silent
Many women endure PIO longer than necessary because they’re afraid to ask.
They worry they’ll sound non-compliant. Or ungrateful. Or difficult.
But suffering is not a requirement for success.
Pain is not proof of effectiveness.
If something hurts every single day, it deserves to be discussed.
How to Have This Conversation With Your Doctor
Instead of asking, “Can I stop PIO?” try asking:
- “Can we check my progesterone levels on vaginal support?”
- “Is combination support an option for me?”
- “Based on my history, is PIO medically necessary or just routine?”
These questions invite collaboration, not confrontation.
A Grounding Truth to Hold Onto
Progesterone doesn’t work because it’s painful.
It works because it reaches the uterus in the right amount.
PIO injections are not the only way to protect a pregnancy.
Vaginal progesterone is not a downgrade.
The goal is support, not suffering.
If your body is bruised and your heart is anxious, you’re allowed to ask for a better way.
Evidence supports it.
Your comfort matters.
And a pregnancy protected with care, not fear, is still a pregnancy worth trusting.