Overview
The scan room goes quiet when the number appears.
6.2 mm.
6.5 mm.
Almost, but not enough.
You nod. You smile. You tell yourself you understand. But inside, frustration tightens its grip.
Why won’t my lining grow?
Why does everything else look fine except this?
Why does my future feel stuck at 7 millimetres?
If you’ve had a cycle delayed or cancelled because your lining didn’t reach the “magic number,” you’re not alone. At a fertility hospital in Chennai, lining-related delays are one of the most emotionally draining parts of treatment.
But here’s the truth most people don’t hear clearly.
Thickness matters.
Timing matters more.
Where the 7mm Rule Came From
The 7mm threshold didn’t come from superstition. It came from observation.
Over time, clinicians noticed that implantation rates improved when the endometrial lining measured around 7 to 8 mm with a healthy pattern. Below that, success rates tended to drop.
So the number became a benchmark.
Not a guarantee.
Not a verdict.
A reference point.
The problem is that reference points often turn into obsessions, especially when cycles depend on them.
What the Uterine Lining Is Actually Doing
The endometrium is not wallpaper. It’s a living, responsive tissue.
Every cycle, it:
- Grows under estrogen
- Develops blood vessels
- Changes its cellular structure
- Becomes receptive for a very specific window
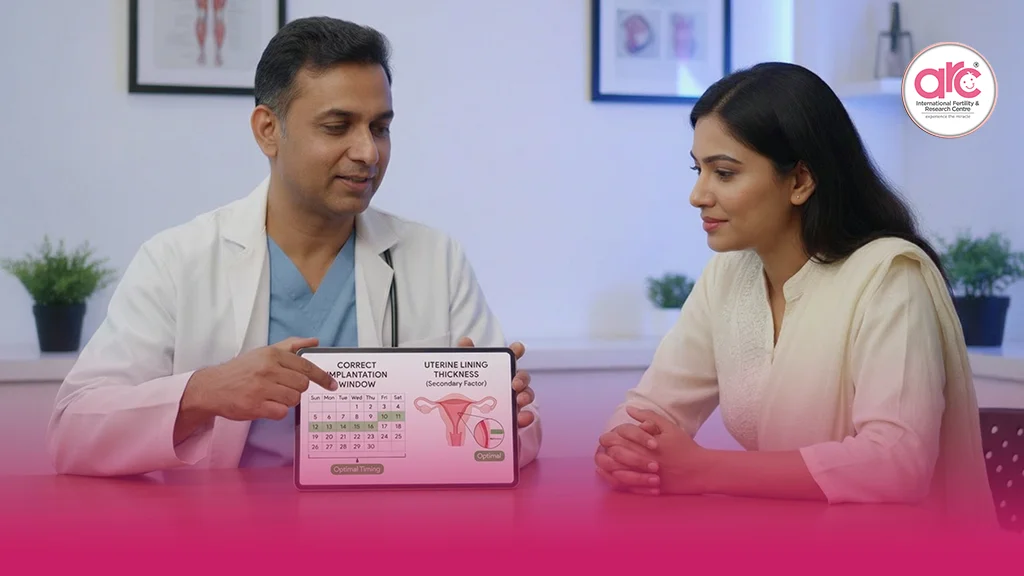
This window is called the Window of Implantation.
It doesn’t stay open long. Usually just a few days.
And here’s the part that changes everything.
A lining can be thick enough but mistimed.
Or slightly thin but perfectly receptive.
Thickness without readiness doesn’t implant well.
Readiness without perfect thickness sometimes does.
Why Timing Often Gets Ignored
Timing is harder to measure than millimetres.
Thickness shows up clearly on ultrasound. Timing lives at a cellular level, invisible to the eye.
This is why patients fixate on numbers. Numbers feel concrete. They feel controllable.
But the uterus doesn’t operate on numbers alone. It operates on rhythm.
At the best fertility hospital in Chennai, doctors increasingly look beyond thickness alone, especially when patients have repeated delays despite good hormone levels.
The Emotional Toll of Lining Delays
A cancelled cycle hurts differently.
It doesn’t come with failure. It comes with suspension.
You did everything right.
You took the medications.
You showed up for scans.
And still, you’re told to wait.
Waiting feels passive, but it’s heavy. It creates doubt about your body, about your future, about whether this will ever line up the way it’s supposed to.
Thin lining is not a sign of weakness. It’s a sign that the uterine environment needs different support, not more pressure.
Why “Pushing” the Lining Doesn’t Always Work
Increasing estrogen isn’t always the answer.
Some linings don’t respond to higher doses because the issue isn’t hormone quantity. It’s blood flow, inflammation, or tissue responsiveness.
This is why some women stay stuck at the same number cycle after cycle, despite escalating medication.
The uterus isn’t being stubborn. It’s being cautious.
Receptivity Is More Than a Measurement
Receptivity means the lining is:
- Well vascularised
- Biochemically ready
- Immunologically calm
- Timed correctly to progesterone exposure
A lining that reaches 7.5 mm too early or too late may be less receptive than a 6.8 mm lining that opens its window at the right moment.
This nuance matters, especially for women who keep missing the “ideal” thickness but feel everything else is aligned.
Where PRP Fits Into This Conversation
For women struggling with persistently thin or unresponsive linings, newer approaches focus on healing rather than forcing.
PRP, Platelet-Rich Plasma, uses the body’s own growth factors to encourage tissue regeneration, blood vessel formation, and cellular responsiveness.
PRP doesn’t just aim to thicken the lining. It aims to improve how the lining behaves.
This is why some women see better implantation outcomes even when thickness improves modestly rather than dramatically.
If you are struggling with a thin lining, explore how we use PRP in IVF to improve endometrial thickness. For the right patients, it can shift the conversation from “why isn’t it growing?” to “is it finally responding?”
Why Cancelled Cycles Are Not Failures
This needs to be said clearly.
A cancelled or delayed cycle is not wasted time.
It’s information.
It tells your care team how your uterus responds, what it needs more of, and what it resists. That data shapes better decisions in the next attempt.
Implantation is too delicate to rush.
Transferring into a lining that isn’t ready doesn’t prove resilience. It risks heartbreak.
What Patients Can Do While Waiting
Waiting doesn’t mean doing nothing.
Supporting receptivity often includes:
- Gentle movement to improve pelvic blood flow
- Reducing inflammation through diet and sleep
- Managing stress that constricts uterine circulation
- Wearing loose, breathable clothing
- Trusting adjustments instead of fighting them
Small changes create internal safety. Safety is what the uterus responds to.
A Reframe That Eases the Anxiety
Instead of asking, “Why won’t my lining reach 7mm?”
Try asking, “What does my lining need to become receptive?”
That shift moves you from blame to collaboration.
Your uterus isn’t behind.
It’s preparing.
A Truth Worth Holding Onto
The 7mm threshold is a guide, not a gate.
Thickness opens the door.
Timing decides whether the door stays open.
When cycles are delayed, it’s not because your body is failing. It’s because implantation is being protected.
Your lining doesn’t need to be perfect.
It needs to be ready.
And readiness, when respected, often arrives quietly, right when it’s meant to.