Overview
Most women don’t hear the word hysteroscopy during a happy phase of life.
It usually enters the conversation after confusion. After months of trying. After bleeding that doesn’t make sense. After IVF failures that come with no explanation except, “Everything looks normal.”
And that’s when the word lands, sounding heavier than it actually is.
Hysteroscopy.
It feels surgical. Invasive. Like something is wrong.
But here’s the truth most women aren’t told early enough.
A hysteroscopy is not about damage.
It is about visibility.
It is one of the few moments in fertility care where the uterus is finally seen, not assumed.
So, What Exactly Is a Hysteroscopy?
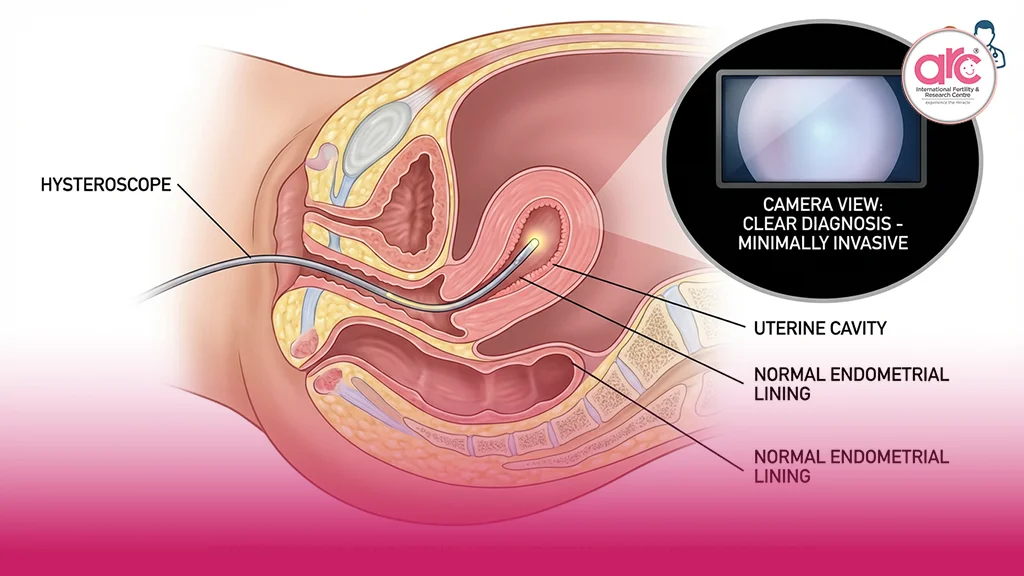
A hysteroscopy is a procedure that allows a doctor to look directly inside the uterus using a thin, flexible camera called a hysteroscope. The camera is gently passed through the vagina and cervix into the uterine cavity.
No cuts.
No incisions.
No blind guessing.
For the first time, the uterine cavity is viewed as it truly is, not as a shadow on an ultrasound screen.
This direct view matters because many uterine problems are small, subtle, and silent. They don’t scream. They whisper. And ultrasounds don’t always hear whispers.
Why Doctors Recommend a Hysteroscopy
A hysteroscopy is never suggested casually. It’s recommended when something doesn’t add up.
Maybe periods are heavier than they should be.
Maybe bleeding appears between cycles.
Maybe IVF transfers keep failing despite good embryos.
Maybe scans look “mostly normal” but pregnancy doesn’t happen.
In these moments, hysteroscopy becomes a clarity tool.
At a fertility hospital in Chennai, hysteroscopy is often used not as a routine step, but as a decisive one, when answers are needed instead of assumptions.
What Can a Hysteroscopy Detect?
The uterus is not an empty room. It is a living space, and small disturbances can change everything.
A hysteroscopy can detect:
Endometrial polyps that block implantation
Submucosal fibroids that distort the cavity
Adhesions or scar tissue from past infections or procedures
Uterine septum or shape abnormalities
Chronic inflammation that affects the lining
Many of these cannot be confirmed reliably through scans alone. They require sight, not interpretation.
Diagnostic vs Operative Hysteroscopy
This distinction matters.
A diagnostic hysteroscopy is purely observational. The doctor looks, assesses, and exits. No tissue is removed. No correction is made. It is often quick and may not even require anesthesia.
An operative hysteroscopy goes a step further. If a polyp, adhesion, or small fibroid is seen, it can often be treated immediately, during the same procedure.
This is one of the reasons hysteroscopy is so powerful. It doesn’t just identify the problem. It often solves it on the spot.
Does a Hysteroscopy Hurt?
This is the question women ask quietly.
The answer depends on the type of hysteroscopy and individual sensitivity. Many diagnostic hysteroscopies cause only mild discomfort, similar to period cramps. Operative procedures may require short anesthesia to ensure comfort.
Pain is not the goal. Precision is.
A best fertility hospital in chennai prioritises patient comfort, not just outcomes. The experience is designed to be controlled, calm, and respectful of the body.
Is Hysteroscopy Safe?
Yes, when performed by experienced hands.
Hysteroscopy is considered a low-risk procedure. Complications are rare, especially when done in specialised settings. The uterus heals quickly. The lining regenerates naturally.
The fear that hysteroscopy damages fertility comes from confusion with older, blind procedures. Modern hysteroscopy is targeted. It removes what doesn’t belong and preserves what does.
In many cases, fertility improves after hysteroscopy, not because the uterus was altered, but because obstacles were removed.
Why Ultrasound Is Not Always Enough
Ultrasound is a valuable tool. But it has limits.
It shows outlines, not textures.
Shadows, not surfaces.
Possibilities, not certainty.
A uterus can look normal on ultrasound and still be hostile to implantation. Tiny polyps, fine adhesions, or subtle inflammation may not register clearly.
Hysteroscopy doesn’t replace ultrasound. It completes the picture.
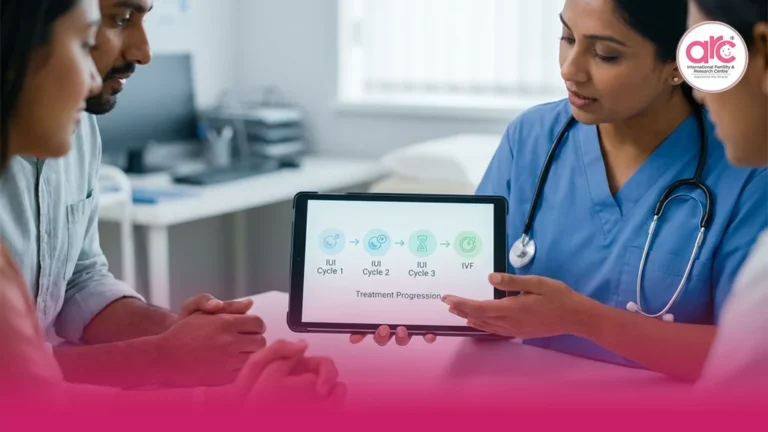
Hysteroscopy and Fertility Treatment
In fertility care, timing matters.
Some women undergo hysteroscopy before IVF. Others are advised after repeated failed transfers. Some conceive naturally afterward. Others proceed with assisted treatment but finally see success.
Hysteroscopy doesn’t guarantee pregnancy. It prepares the ground.
For women with unexplained infertility, it often answers the question they’ve been asking for years, “Why isn’t this working?”
Emotional Weight Around the Procedure
Let’s acknowledge something medical articles often ignore.
The uterus carries emotional weight. It’s tied to identity, motherhood, loss, and expectation. Any procedure involving it can feel personal, even threatening.
Fear doesn’t mean weakness. It means investment.
But fear should not be fed by silence. Understanding what hysteroscopy is and isn’t allows women to approach it with agency instead of anxiety.
What Hysteroscopy Is Not
It is not major surgery.
It is not a punishment for infertility.
It is not a last resort.
It is a tool for truth.
When the uterus is seen clearly, treatment becomes honest. Guesswork reduces. And decisions become grounded in reality, not hope alone.
The Bigger Picture
A hysteroscopy doesn’t change who you are. It doesn’t reduce your chances. It doesn’t make the uterus weaker.
In many cases, it does the opposite.
It gives the uterus a fair chance to function as it should.
And sometimes, that’s all the body was waiting for.
Final Thought
Hysteroscopy is not about finding something wrong.
It’s about making sure nothing important is missed.
In a fertility journey filled with waiting, ambiguity, and silent disappointment, seeing clearly is an act of respect, for the body and for the woman carrying the questions.
The uterus is not fragile.
It is resilient.
And when it is finally understood, it often responds in ways that surprise even medicine.